Thermography for Breast Health, Prevention
What is Thermography?
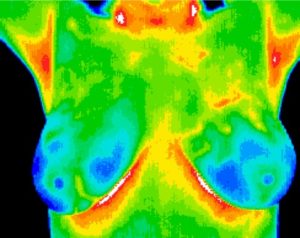
Thermography is essentially a photograph of the heat produced by the body. The body is constantly emitting heat as infrared radiation from its surface. A thermographic camera takes a picture of these rays. Areas of the body that are more metabolically active and have more blood flow will produce more infrared rays and will be visible on the thermogram. Once pictures are taken they are then analyzed by a board certified thermologist. The most common use of thermography is for breast health screening. Thermography is a wonderful tool for assessing physiological changes associated with fibrocystic breast disease, mastitis, mammary dysplasia and metabolically active tissue. We use state-of-the-art Digital Infrared breast imaging and comprehensive treatment protocols to help women of all ages maintain healthy breasts for long and healthy lives. Our high-quality radiometric camera, strict quality control guidelines and highly accurate interpretation service are the best around. Take advantage of this wonderful resource!
History
1982 FDA approved: Thermography was approved as an adjunctive diagnostic breast cancer screening procedure.
1950’s to present: Thermography for the purpose of breast screening has undergone extensive research since the late 1950’s with more than 1000 peer-reviewed studies published in the medical literature.
What are the benefits of Thermography?
Breast health screening: Thermography is a wonderful tool for identifying breast conditions in women of all sizes, as well as young women, women with implants and conditions such as fibrocystic breast disease and mastitis two easily reversed conditions.
Prevention: Breast Cancer is the second-leading cause of death among women. Thermography can detect first signs that breast cancer may be forming – up to 10 years earlier than any other procedure. Earlier detection means there is time for prevention. Implementing comprehensive treatment can result in reversal of these changes and prevention.
No radiation or other risk to your health: Thermography is entirely safe since the camera is only receiving information from your body and does not itself emit anything.
No compression of the breast tissue: Thermography does not involve the painful compression of breast tissue.
Monitor your progress: See the results of your treatment without the use invasive and harmful radiation.
Mammography Compared to Thermography
A mammogram uses radiation to detect the internal anatomical structure of the breast. It is still considered the ‘Gold Standard’ for early detection of breast cancer. Thermography detects the infrared emitted from the body surface to measure the physiological changes occurring within the breasts. Mammography has led to earlier detection of breast cancer leading to a 30-40% reduction in mortality rates from breast cancer. When thermography and mammography are used together the detection of breast cancer increases by 10%. Ideally, we would use thermography to monitor physiological changes in women’s breasts allowing for preventative treatment and mammography to confirm significant findings and guide diagnosis of significant disease.
How is breast cancer diagnosed?
Thermography and mammography help direct us to where breast tissue appears to be abnormal. However, neither thermography or mammography can be used to diagnose breast cancer, they are screening tools used to detect tissue changes associated with breast cancer. Breast cancer can only be diagnosed by biopsy of breast tissue. Any suspect tissue is captured by a needle and is then visualized under a microscope to look for cellular changes consistent with cancer. If significant abnormalities are seen on thermogram we will then refer you for a mammogram and/or biopsy.
References
Acharya, U. R., E. Y. Ng, et al. (2010). “Thermography Based Breast Cancer Detection Using Texture Features and Support Vector Machine.” J Med Syst.
Anderson, J. (2010). “Thermography: a holistic approach to breast screening.” Beginnings 30(1): 12-3.
Arora, N., D. Martins, et al. (2008). “Effectiveness of a noninvasive digital infrared thermal imaging system in the detection of breast cancer.” Am J Surg 196(4): 523-6.
Brodersen, J., K. J. Jorgensen, et al. (2010). “The benefits and harms of screening for cancer with a focus on breast screening.” Pol Arch Med Wewn 120(3): 89-94.
Christiansen, C. L., F. Wang, et al. (2000). “Predicting the cumulative risk of false-positive mammograms.” J Natl Cancer Inst 92(20): 1657-66.
Clark, R. M. (1983). “Thermography.” CA Cancer J Clin 33(6): 370-2.
Elmore, J. G., M. B. Barton, et al. (1998). “Ten-year risk of false positive screening mammograms and clinical breast examinations.” N Engl J Med 338(16): 1089-96.
Gautherie, M. and C. M. Gros (1980). “Breast thermography and cancer risk prediction.” Cancer 45(1): 51-6.
Gershon-Cohen, J. (1967). “Mammography, thermography and xerography.” CA Cancer J Clin 17(3): 108-12.
Gotzsche, P. C. and O. Olsen (2000). “Is screening for breast cancer with mammography justifiable?” Lancet 355(9198): 129-34.
Haberman, J. D. (1968). “The present status of mammary thermography.” CA Cancer J Clin 18(6): 315-21.
Head, J. F., F. Wang, et al. (1993). “Breast thermography is a noninvasive prognostic procedure that predicts tumor growth rate in breast cancer patients.” Ann N Y Acad Sci 698: 153-8.
Holloway, C. M., A. Easson, et al. (2010). “Technology as a force for improved diagnosis and treatment of breast disease.” Can J Surg 53(4): 268-77.
Isard, H. J. (1976). “Cancer in the “cold” breast thermogram.” AJR Am J Roentgenol 127(5): 793-6.
Isard, H. J., W. Becker, et al. (1972). “Breast thermography after four years and 10000 studies.” Am J Roentgenol Radium Ther Nucl Med 115(4): 811-21.
Johns, L. E. and S. M. Moss (2010). “False-positive results in the randomized controlled trial of mammographic screening from age 40 (“Age” trial).” Cancer Epidemiol Biomarkers Prev 19(11): 2758-64.
Kennedy, D. A., T. Lee, et al. (2009). “A comparative review of thermography as a breast cancer screening technique.” Integr Cancer Ther 8(1): 9-16.
Kontos, M., R. Wilson, et al. (2011). “Digital infrared thermal imaging (DITI) of breast lesions: sensitivity and specificity of detection of primary breast cancers.” Clin Radiol 66(6): 536-9.
Lee, P., K. K. Ho, et al. (2011). “Hot fat in a cool man: infrared thermography and brown adipose tissue.” Diabetes Obes Metab 13(1): 92-3.
Njor, S. H., A. H. Olsen, et al. (2007). “Predicting the risk of a false-positive test for women following a mammography screening programme.” J Med Screen 14(2): 94-7.
Oliver, C. (1977). “Thermography, a Canadian invention finding wider applications.” Can Med Assoc J 117(6): 680, 683-5.
Parisky, Y. R., A. Sardi, et al. (2003). “Efficacy of computerized infrared imaging analysis to evaluate mammographically suspicious lesions.” AJR Am J Roentgenol 180(1): 263-9.
Plotnikoff, G. and T. Carolyn (2009). “Emerging controversies in breast imaging: is there a place for thermography?” Minn Med 92(12): 37-9, 56.
Salhab, M., L. G. Keith, et al. (2006). “The potential role of dynamic thermal analysis in breast cancer detection.” Int Semin Surg Oncol 3: 8.
Sterns, E. E. and B. Zee (1991). “Thermography as a predictor of prognosis in cancer of the breast.” Cancer 67(6): 1678-80.
Sterns, E. E., B. Zee, et al. (1996). “Thermography. Its relation to pathologic characteristics, vascularity, proliferation rate, and survival of patients with invasive ductal carcinoma of the breast.” Cancer 77(7): 1324-8.
Wang, J., K. J. Chang, et al. (2010). “Evaluation of the diagnostic performance of infrared imaging of the breast: a preliminary study.” Biomed Eng Online 9: 3.
Williams, K. L., B. H. Phillips, et al. (1990). “Thermography in screening for breast cancer.” J Epidemiol Community Health 44(2): 112-3.